Extending stem cell compatibility with antibodies

Donor compatibility is one of the biggest bottlenecks associated with hematopoietic stem cell transplants. In this study, researchers explore the idea of using antibodies as a way of preparing patients to receive stem cells from imperfectly matched donors.
What is a hematopoietic stem cell transplant?
Hematopoietic stem cells (HSCs) are early-stage cells that give rise to all other types of blood cells in the body. These cells found in the bone marrow are responsible for replenishing trillions of blood cells necessary to keep us going. Cord blood is another source of hematopoietic stem cells, which is found in the umbilical cord after birth.
During a hematopoietic stem cell transplant, sometimes also referred to as a bone marrow transplant or simply a stem cell transplant, HSCs from a donor are collected and transplanted into a patient with a blood disorder. The idea is to replace the diseased stem cells of a patient with healthy donor stem cells to treat a disease.
To date, HSC transplants are used to treat genetic blood disorders like sickle cell anemia and thalassemia, autoimmune diseases, and certain types of cancers.
Barriers to overcome
Even though HSC transplants save lives, the procedure is not without its risks and difficulties.
Problem #1- The need to precondition
Before receiving a transplant, the body of a patient has to be preconditioned or prepared to receive donor stem cells. This process requires removing their bone marrow, blood cells, and immune cells, usually using chemotherapy, radiation, or both. The issue is, these methods are quite harsh on the body, which is why doctors often offer transplants as a last resort.
Problem #2 – Matching donor cells
Donor stem cells usually consist of a mixture of cells, not just hematopoietic stem cells. As a result, immune cells from the donor are transferred into the patient, which in some cases leads to a life-threatening complication called the graft-versus-host disease. In this case, a type of immune cell called T cells from the donor recognizes the patients’ cells as foreign and starts attacking them. The likelihood of graft-versus-host disease can be reduced by closely matching the donor stem cells to patients.
Finding this perfect match can be extremely difficult, mostly if the patient belongs to an ethnic minority, which means immunosuppressive drugs are necessary to minimize the risk of rejection. The issue here is that while these drugs increase the likelihood of engraftment (the donor stem cells being incorporated into the patients’ bone marrow), they also increase the risk of infections.
Antibodies to the rescue
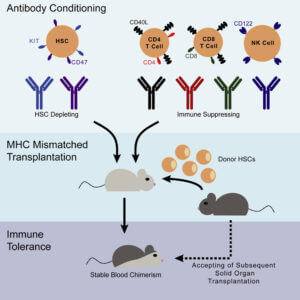
In this study, the researchers are proposing to overcome both these difficulties using antibodies.
Antibodies are proteins made by the immune system. They recognize markers on the surface of foreign bodies (called antigens) and signal the immune system to attack and destroy these intruders. In their previous work, these researchers show that introducing antibodies specific to HSCs and immune cells in mice can facilitate the transplant of mismatched donor samples.
The idea is when introduced into patients, these antibodies recognize and selectively destroy the HSCs using a process called antibody-mediated depletion, allowing new HSCs from the donor to take their place. While these experiments addressed the issue of harsh preconditioning methods, they did not tackle the need to find matching donor samples, which was the purpose of this current study.
Using mismatched donor samples
Here, the researchers extended their previous method by including additional antibodies to target immune cells. The cocktail of six antibodies used contained two specific to HSCs and four specific to various immune cells.
They were able to successfully transplant mice preconditioned with the antibody cocktail with HSCs that were only half-matched (haploidentical) to the recipient mice. A haploidentical transplant would be similar to a transplant that happens between a parent and a child, or between siblings, when there is only a 50% match between the donor and recipient immune markers (HLA matching).
What’s more, using their method, they were able to perform transplants between fully mismatched donor and recipient mice successfully.
Looking to the future
The logical next step for these researchers will be to perform similar experiments in larger animal models to substantiate the finding that antibody-mediated preconditioning can be reproduced in other model systems.
And, if it does (we hope it does), what it means for us would be that one day it would pave the way to:
- Safe, gentle transplants involving hematopoietic stem cells
- Using “half-matched” stem cells from parents and sibling to treat disease
- Using lab-grown stem cells as an alternative for treating diseases
As we mentioned already, finding matching stem cells is one of the significant bottlenecks associated with HSC transplants. So, any method that can increase the availability of organs and stem cells would most definitely be welcomed.
Reference
George, BM, Kao, KS, Kwon H. et al (2019) Antibody Conditioning Enables MHC-Mismatched Hematopoietic Stem Cell Transplants and Organ Graft Tolerance. Cell Stem Cell 25, 185–192. Doi: https://doi.org/10.1016/j.stem.2019.05.018.
Related Posts

Novel Cord Blood Stem Cell Treatment Leads to HIV Remission


Stem Cell Transplantation Shows Potential in Stroke Recovery