Stem cells to beta cells: Treating type 1 diabetes with converted stem cells

Hope for personalized treatment, as researchers convert human stem cells into insulin-producing beta cells using small molecules
In 1921, two Canadian scientists managed to isolate insulin, a discovery that transformed type 1 diabetes from a terminal illness to a treatable disease. While insulin was an amazing treatment option, it is not a cure for diabetes. This is why in the past few decades, researchers around the world have been hunting for a cure for diabetes. Here we highlight a study that brings us another step closer to a cure where scientists have produced insulin-making pancreatic cells from stem cells in the lab.
A brief look at Type 1 diabetes
Type 1 diabetes is an autoimmune disease when a person’s immune system attacks and destroys the beta cells of the pancreas. Beta cells are responsible for making and releasing insulin, the hormone that controls the sugar levels in our blood. People with type 1 diabetes are unable to make insulin, which makes them completely reliant on insulin injections for controlling blood sugar levels.
A cure instead of a treatment
With automated insulin delivery systems and minimally invasive blood sugar monitoring devices that send results to a cell phone, we have indeed come a long way in effectively treating diabetes. But even with these interventions, people with type 1 diabetes must live a carefully controlled lifestyle and their life expectancy is 12 years less than someone without the conditions. Therefore, it is important to find ways to restore beta cell function inside the body, so insulin can be made in response to sugar levels.
Making beta cells in the lab
Stem cells, for obvious reasons, are the top candidate being explored for cell therapies involving type 1 diabetes. Stem cells can grow almost indefinitely and can be converted into a whole range of different types of cells in the body with the right signal. However, uncovering the signals that will drive a stem cell to become a beta cell has not been a small feat. Furthermore, determining just how much signal to provide these cells and for how long has also been challenging.
Many studies to date have focused on using growth factors, substances that promote stem cells to produce other types of cells, to produce beta cells. But since growth factors are expensive and unstable, their use can be too costly and inefficient for manufacturing making the product non-affordable.
Effective and affordable
Here is where the current study comes in. These researchers took a different approach replacing growth factors with a cocktail of small molecules discovered in their lab to stimulate stem cells. According to the lead author of the study “[the] small molecules are much cheaper and far more stable than growth factors, and [they] still emulate the effect of growth factors..”
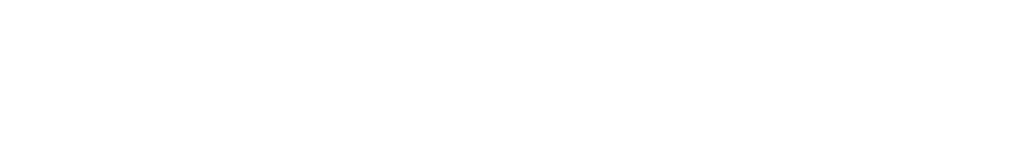
 Generating beta cells from stem cells.
Generating beta cells from stem cells.
Adapted from Jiang et al (2021).
Their cocktail had a chemical compound the lab designated as CHIR99021 (CHIR)). CHIR activated a signaling pathway in the cells that directed cells to differentiate into other cell types.
But here is where it got tricky. If the CHIR fully activated the signaling pathway, stem cells went on to make mature heart cells. But if they used an intermediate dose to partially activate this pathway, stem cells generated a cell that could be coaxed into becoming a mature pancreatic beta cell. As you can imagine years of hard work went into determining the “intermediate” dose of CHIR that should be used.
Onwards and upwards
Once they had mature beta cells, researchers went on to test their functionality. They found that the lab-derived beta cells can sense sugar levels in the environment and produce insulin. The group will next move on uncovering an effective way to deliver these lab-made cells to patients in a way that the patients’ immune system will not destroy these cells. Once this can be done, they will move onto clinical trials for testing their effectiveness.
It may be years before these chemically coaxed beta-cells may be transplanted into patients to cure diabetes. But we can celebrate the fact this new process may make cell therapy more cost-effective that when the day comes everyone who needs it can afford it.
Reference
Jiang et al., Generation of pancreatic progenitors from human pluripotent stem cells by small molecules, Stem Cell Reports (2021), https://doi.org/10.1016/j.stemcr.2021.07.021
Related Posts

Novel Cord Blood Stem Cell Treatment Leads to HIV Remission


Stem Cell Transplantation Shows Potential in Stroke Recovery